Irritable bowel syndrome (IBS) is a chronic gastrointestinal disorder affecting millions worldwide, causing discomfort, irregular bowel habits, and reduced quality of life. IBS symptoms such as intestinal discomfort, gut bloating, and bowel pain can interfere with daily routines and overall well-being.
At our Altus Emergency Room, Lumberton, TX, we understand the stress and frustration IBS can bring. Every patient’s experience is unique, and recognizing the variety of triggers and symptom patterns is essential for effective management and lasting relief.
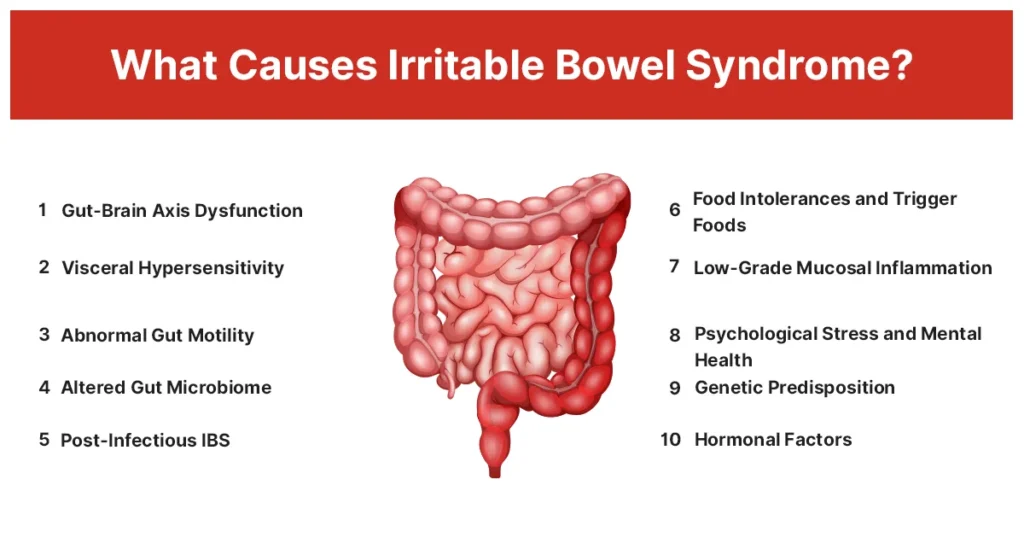
What Causes IBS
The exact cause of IBS disease isn’t fully understood, but it often involves gut-brain communication issues, abnormal intestinal motility, and changes in the gut microbiome. Stress, infections, and certain foods can trigger IBS flare-ups, leading to intestinal discomfort, bloating, and irregular bowel habits. A study found that about 10% of people developed IBS within a year after a gastrointestinal infection, highlighting post-infectious causes as an important factor.
1. Gut-Brain Axis Dysfunction
Disruption between the brain and the gut can alter bowel movements and pain perception, causing abdominal pain, bloating, and irritable bowel reflux. This dysfunction may trigger IBS flare-ups and worsen digestive issues during periods of stress. Gut-brain communication irregularities are common in IBS, especially during anxiety or emotional tension.
Treatment
- Cognitive Behavioral Therapy (CBT): Reduces stress-related gut symptoms.
- Neuromodulators: (e.g., low-dose amitriptyline or SSRIs) to improve gut-brain signaling.
- Mindfulness and relaxation techniques to control stress-induced flare-ups.
- Regular exercise helps maintain proper intestinal motility and reduces the impact of stress.
2. Visceral Hypersensitivity
IBS patients may feel discomfort from normal intestinal activity due to heightened gut sensitivity. Even small amounts of gas or stool can cause painful bowel movements, bloating, or irritable bowel reflux. This heightened sensitivity is particularly noticeable during IBS flare-ups or after consuming trigger foods, explaining why symptoms vary among patients.
Treatment
- Antispasmodic medications (e.g., dicyclomine, hyoscyamine) to relieve intestinal spasms.
- Low-dose antidepressants (e.g., tricyclics) to reduce nerve sensitivity in the gut.
- Heat therapy: Warm compresses or heating pads to relax abdominal muscles.
- Relaxation exercises, such as deep breathing or yoga, can help calm visceral nerves.
3. Abnormal Gut Motility
Irregular intestinal muscle contractions can cause diarrhea, constipation, or alternating patterns (constipation after diarrhea) in IBS patients. These contractions contribute to gut bloating, abdominal discomfort, and digestive issues. Both fast and slow motility affect stool consistency and nutrient absorption, making it important to identify the underlying motility pattern.
Treatment
- Laxatives (e.g., polyethylene glycol) for constipation-predominant IBS.
- Antidiarrheal medications (e.g., loperamide) for diarrhea-predominant IBS.
- Dietary fiber adjustments: soluble fiber for constipation, limiting insoluble fiber for diarrhea.
- Adequate hydration and regular meal patterns to normalize bowel movements.
4. Altered Gut Microbiome
Imbalances in gut bacteria can lead to bloating, gas, and digestive disturbances, triggering IBS flare-ups. Dysbiosis may worsen irritable bowel reflux and sensitivity to certain foods. Many patients notice improvement when the microbiome is restored through diet or supplements. A balanced microbiome supports regular bowel movements and reduces bowel pain.
Treatment
- Probiotics (e.g., Bifidobacterium infantis 35624) to restore healthy bacteria.
- Prebiotics to nourish beneficial gut microbes.
- Targeted antibiotics (e.g., rifaximin) for small intestinal bacterial overgrowth (SIBO).
- Balanced diet rich in fiber and fermented foods to support gut health.
5. Post-Infectious IBS
IBS may develop after gastrointestinal infections like gastroenteritis, food poisoning, or severe diarrhea. Symptoms often include bloating, abdominal pain, and alternating constipation and diarrhea. Post-infectious changes in gut motility and microbiome can persist, sometimes triggered by medications such as antibiotics. Patients may notice flare-ups after minor dietary or stress triggers.
Treatment
- Hydration and electrolyte replacement during and after infections.
- Probiotics to restore gut microbial balance.
- Anti-diarrheal or anti-spasmodic medications for symptom relief.
- Gradual reintroduction of normal diet with low-FODMAP foods to minimize flare-ups.
6. Food Intolerances and Trigger Foods
Certain foods, such as fatty, spicy, or high-FODMAP items, can provoke IBS flare-ups, bloating, or irritable bowel reflux. Reactions vary between individuals, making it essential to identify personal ibs trigger foods. Food intolerance can worsen bowel pain and contribute to digestive instability.
Treatment
- Elimination diets under guidance to identify triggers.
- Low-FODMAP diet to reduce gas and bloating.
- Gradual reintroduction of foods to test tolerance.
- Smaller, frequent meals to reduce intestinal stress.
7. Low-Grade Mucosal Inflammation
Subtle gut inflammation or increased intestinal permeability (“leaky gut”) can worsen gut bloating, abdominal pain, and digestive problems. Inflammation heightens sensitivity and prolongs IBS flare-ups, especially in diarrhea-predominant or post-infectious IBS. Addressing inflammation can improve gut function and reduce symptoms.
Treatment
- Anti-inflammatory diet: limit processed foods, sugar, and alcohol.
- Supplements like zinc, carnosine, or glutamine for gut barrier support.
- Avoid irritants such as caffeine or alcohol.
- Stress-reduction techniques to limit cortisol-induced inflammation.
8. Psychological Stress and Mental Health
Stress, anxiety, and depression can worsen digestive issues and trigger IBS flare-ups. These factors influence gut motility and sensitivity, contributing to painful bowel movements, bloating, and gut discomfort. Mental health management is crucial to reduce the frequency and severity of symptoms.
Treatment
- Cognitive Behavioral Therapy (CBT) to manage stress-related triggers.
- Mindfulness meditation and relaxation exercises for symptom control.
- Medications for anxiety or depression, if indicated (SSRIs, SNRIs).
- Regular exercise and sufficient sleep to maintain gut-brain balance.
9. Genetic Predisposition
IBS disease can run in families, increasing susceptibility to flare-ups, gut bloating, and painful bowel movements. Genetics may influence gut-brain communication, intestinal sensitivity, and response to ibs trigger foods. Awareness of family history allows early symptom management and preventive strategies.
Treatment
- Monitor early signs of gastrointestinal disease in at-risk individuals.
- Lifestyle and dietary adjustments to prevent symptom onset.
- Regular medical check-ups for timely interventions.
- Tailored management strategies with healthcare providers.
10. Hormonal Factors
IBS affects women more frequently than men, likely due to hormonal fluctuations affecting gut motility and sensitivity. IBS symptoms in females often worsen during menstrual cycles, triggering gut discomfort, bowel pain, and bloating. Recognizing hormonal influence helps personalize treatment and symptom management.
Treatment
- Track symptoms in relation to menstrual cycles.
- Adjust diet and stress management during high-risk periods.
- Gentle exercise and fiber-rich meals to support bowel function.
- Consult a gynecologist or gastroenterologist for persistent symptoms.
Warning Signs You Should Not Ignore
While many IBS symptoms can be managed at home, certain warning signs may indicate a more serious condition requiring urgent medical attention. Persistent or severe changes in bowel habits, sudden abdominal pain, or unexplained systemic symptoms should not be overlooked.
- Blood in stool or black, tar-like stool.
- Significant, unintentional weight loss.
- Persistent fever, night sweats, or severe fatigue.
- Sudden worsening of abdominal muscle deficiency syndrome or severe abdominal discomfort.
If you experience any of these warning signs, contact Altus Emergency Centers immediately for prompt evaluation.
IBS Curable?
No, IBS currently has no cure. With proper management, patients can achieve effective ibs relief and reduce flare-ups. Identifying ibs trigger foods and stress patterns allows targeted treatment. Combining medical therapy, lifestyle changes, and mental health support helps minimize bowel pain, bloating, and digestive issues.
Altus Emergency Centers: Fast Support for IBS Symptoms
If you experience severe abdominal pain, sudden changes in bowel habits, or persistent bloating, timely care can make all the difference. What causes irritable bowel syndrome may vary, but when symptoms escalate or become unmanageable, early evaluation helps prevent complications and provides relief.
At Altus Emergency Centers, our team offers trusted emergency care for severe or persistent IBS symptoms. From abdominal discomfort to painful bowel movements or sudden IBS flare-ups, prompt assessment and targeted treatment ensure safe recovery and peace of mind.