Many people notice changes in their nasal or throat secretions and wonder, “Why is my mucus yellow?” Yellow mucus can be concerning, especially when it’s thick or persistent. In most cases, it shows that your body is responding to infection, irritation, or inflammation. Understanding the cause helps you determine when it’s normal and when medical attention may be needed.
Whether you see thick yellow mucus, yellow mucus from the throat, or yellow nasal phlegm, it’s important to identify the underlying reasons. If your symptoms feel severe or unusual, our emergency room in Waxahachie is ready to provide quick evaluation and care.
What Does Yellow Mucus Mean?
Yellow mucus indicates your immune system is actively fighting infections. White blood cells mix with mucus, giving it a yellow hue. This often occurs during viral infections, mild bacterial infections, or airway irritation. A study found that about 12% of yellow or green mucus cases were linked to bacterial infections.
What Does Yellow Mucus Indicate?
Yellow mucus reflects your body’s active response to infection, inflammation, or irritation. It occurs when immune cells mix with mucus to trap pathogens. Often, it appears during colds, sinus irritation, or mild infections. Persistent or worsening yellow mucus may require professional medical evaluation.
Also Read: Why Is My Mucus Black
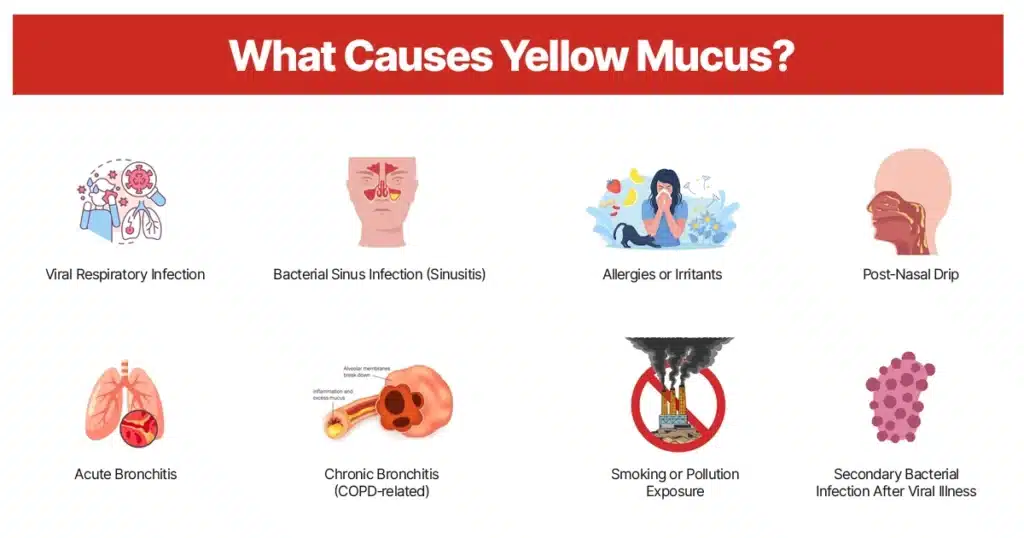
What Causes Yellow Mucus?
Yellow mucus is a symptom that your body is responding to infections or irritants. Immune cells mix with mucus to trap bacteria, viruses, or allergens, giving it a yellow color. This hue reflects your body’s natural defense mechanisms. Identifying the cause helps determine the right treatment and care.
Viral Respiratory Infection
Viruses like the common cold or flu are the most frequent cause of thick yellow mucus. White blood cells flood the infected area, mixing with mucus and giving it a yellow tint. Symptoms usually improve within 7–10 days without antibiotics. Supportive care, like hydration, rest, and over-the-counter remedies, can help with recovery.
Symptoms:
- Runny or stuffy nose with post-nasal drip.
- Yellow mucus from my throat.
- Yellow nasal phlegm.
- Mild fatigue.
- Low-grade fever.
Bacterial Sinus Infection (Sinusitis)
Bacterial infections in the sinuses can cause dark yellow mucus or green and yellow snot. Thickened mucus results from immune cells fighting bacteria in the sinus cavities. Symptoms often worsen after a week of a cold. Medical evaluation is recommended to determine if antibiotics are necessary.
Symptoms:
- Facial pressure or pain around the eyes or cheeks.
- Persistent nasal congestion.
- Yellow liquid from the nose.
- Reduced sense of smell.
- Bad breath.
Learn More About: When to Visit ER for Sinus Infections
Allergies or Irritants
Although allergies often produce clear mucus, prolonged exposure to dust, pollen, or smoke can lead to yellow mucus in the throat or nose. The color change is caused by immune cells reacting to irritants. Avoiding triggers reduces mucus production. Antihistamines or nasal sprays may relieve symptoms.
Symptoms:
- Sneezing and an itchy nose.
- Watery or red eyes.
- Nasal congestion without fever.
- Thick yellow mucus from the nose.
- Seasonal flare-ups.
Post‑Nasal Drip
Excess mucus may drip down the back of the throat, appearing as yellow mucus in the throat, especially at night. This occurs when mucus production increases due to infection, allergies, or sinus irritation. It can cause throat discomfort and persistent coughing. Treating underlying triggers reduces post-nasal drip.
Symptoms:
- Frequent throat clearing.
- Nighttime cough or throat irritation.
- Sore throat.
- Sensation of mucus accumulation.
Acute Bronchitis
Inflammation of the bronchial tubes produces yellow phlegm color, often with a productive cough. White blood cells mix with mucus to combat infection. Symptoms typically follow a viral illness and resolve within a few weeks. Supportive care, including rest, fluids, and symptom management, is recommended.
Symptoms:
- Cough producing yellow phlegm color.
- Mild chest discomfort.
- Low-grade fever.
- Wheezing or shortness of breath.
Chronic Bronchitis (COPD‑related)
Chronic bronchitis causes persistent airway inflammation and regular production of green and yellow snot or thick yellow mucus from the nose and lungs. Accumulated mucus triggers frequent coughing. This is common in smokers or those with COPD. Medical management helps control symptoms and prevent flare-ups.
Symptoms:
- Daily cough with discolored mucus.
- Shortness of breath on exertion.
- Recurrent respiratory infections.
- Fatigue or low energy.
Read About: How to Survive Bronchitis
Smoking or Pollution Exposure
Long-term exposure to smoke or environmental toxins irritates the airways, leading to dark yellow mucus. Chronic irritation triggers inflammation and increased mucus production. Avoiding pollutants can improve mucus color and respiratory health. Supportive care reduces symptoms and aids mucus clearance.
Symptoms:
- Persistent cough with thick yellow mucus.
- Chest tightness or discomfort.
- Shortness of breath during activity.
- Frequent throat clearing.
Secondary Bacterial Infection After Viral Illness
A bacterial infection following a viral illness can worsen or prolong yellow or green mucus. White blood cells and bacteria mix in the mucus, causing thick discoloration. Prompt evaluation ensures proper treatment with antibiotics if needed. Early care prevents complications like sinus or lung infection.
Symptoms:
- Symptoms worsening after initial improvement.
- Fever returning after a cold.
- Yellow nasal phlegm thickens.
- Increased sinus pressure or discomfort.
When to See a Doctor
Yellow mucus often resolves on its own, but persistent or severe symptoms require medical attention. Early evaluation prevents complications and ensures proper treatment. Seek care if your symptoms are unusual, worsening, or accompanied by additional warning signs. See a healthcare provider if you have:
- Symptoms lasting more than 10–14 days.
- High fever or worsening symptoms.
- Shortness of breath or chest pain.
- Nasal blood mucus or coughing up blood.
- Confusion or severe fatigue.
If these signs appear, contact the Altus Emergency Centers for timely care.
Yellow Mucus Treatment
Treatment depends on the underlying cause. Most cases improve with supportive care, hydration, and symptom management. Interventions aim to thin mucus, reduce inflammation, and clear infections effectively. Common treatment options include:
- Decongestants: Reduce nasal swelling and relieve thick yellow mucus from the nose.
- Saline Nasal Rinses: Help thin mucus and clear nasal passages.
- Expectorants (E.G., Guaifenesin): Make coughs more productive by thinning yellow phlegm color.
- Antihistamines: Treat allergy-related mucus production.
- Humidifiers: Moist air helps thin mucus and ease congestion.
- Rest And Hydration: Support immune function and mucus clearance.
- Antibiotics: Only if bacterial infection is confirmed.
- Inhaled Bronchodilators Or Steroids: For bronchitis or COPD flare-ups.
- Avoid Irritants: Such as smoke or pollution.
- Warm Fluids: Tea, broth, or water helps soothe the throat and thin mucus.
Altus Emergency Centers: Expert Care for Yellow Mucus
Are you wondering, “Why is my mucus yellow?” or noticing thick yellow phlegm color, post-nasal drip, or persistent coughing? At Altus Emergency Centers, our medical team provides fast evaluation to identify the cause and guide proper treatment. Early care helps prevent complications and ensures effective management of infections or irritation.
If your symptoms worsen or include fever, chest discomfort, or shortness of breath, Altus Emergency Center provides compassionate emergency care. We monitor yellow nasal phlegm and offer personalized treatment for safe, speedy recovery.

